Reimbursement Consulting
The Service: Analysis of Payor Trends in Reimbursement +
Projections of Future Payor Rates
What We Do
- Define key business need(s)
- Conduct primary and secondary research
-
- We can design and conduct 1-on-1 or group interviews with industry leaders
- We also research publicly available information and reports
-
- Develop value messaging for products reflecting key business needs and market trends
What to Expect
- A comprehensive analysis of current
- Payor coverage dynamics
- Coding strategy
- Pricing pressures
- A workplan designed to secure payer acceptance of your Reimbursement modeling
- Development of collateral supporting advocacy efforts with payors
The Case Study: Reimbursement Consulting
The Situation
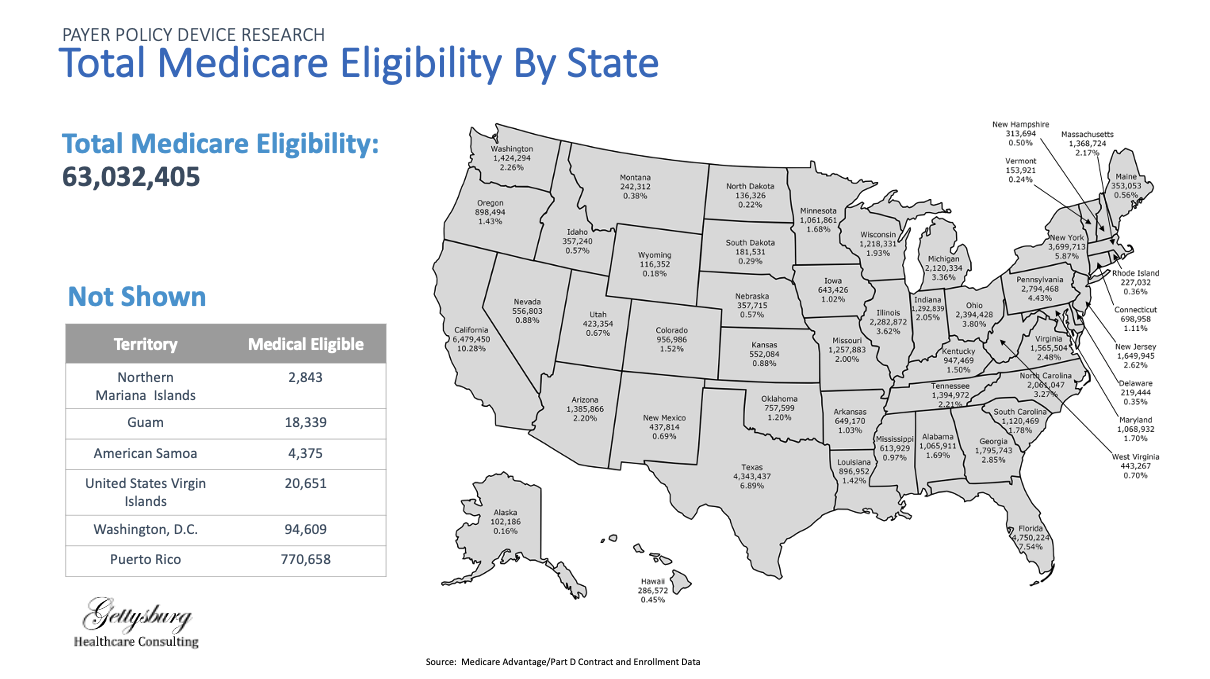
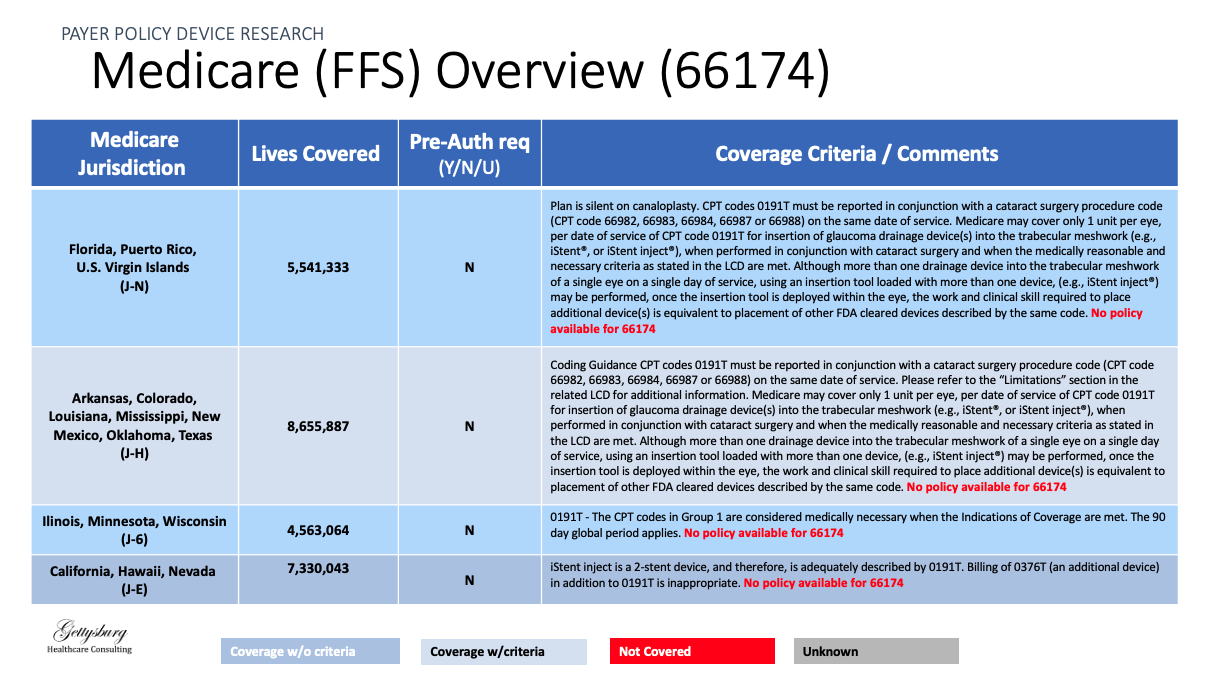
Gettysburg Healthcare Consulting was engaged by a developer of a novel ophthalmic product to identify changes in reimbursement trends
The Ask
Our client wanted to understand how enrollment growth in different payor plans (e.g., Medicare Advantage) was trending and what those changes could mean for their product
The Actions
Payor Trend Review
Reviewed and performed primary and secondary research to identify enrollment and spending trends in different payors
Coverage Pathways
Identified trends and determined possible implications of payor growth in different markets on client’s product
Representative Deliverables: Reimbursement Consulting